

Paula Montana De La Cadena, M.D., a cardiologist at Baptist Health Miami Cardiac & Vascular Institute
When 18-year-old Sirikorn “Jamsai” Unsri (“Jamsai” to his friends) walked into his pediatrician’s office for a routine annual checkup, he expected nothing more than the usual reminders about maintaining his health and vision as he looked ahead to graduating from high school and heading off to his first year of college.
Instead, after the doctor listened to his patient’s heart, he removed his stethoscope, called Jamsai’s parents into the exam room and said, “I hear something with his heart I’m concerned about.”
Within days, tests confirmed the unimaginable. Jamsai had a large atrial septal defect (ASD), a hole in the wall that separates the two upper chambers of the heart. According to the American Heart Association, ASD is among the most common congenital heart defects, affecting about one in every 100 people.
In infants and children, ASD is often detected early but sometimes, as in Jamsai’s case, it can go unnoticed until young adulthood. Left untreated, the hole causes blood to flow abnormally between the heart’s chambers. Over time, this extra burden on the heart can cause arrhythmias, shortness of breath and even congestive heart failure.
“I was about to graduate high school, about to turn 18,” Jamsai recalls. “To hear that I had a hole in my heart rattled my world. My whole life felt like it was crumbling.”
(Watch now: The last thing 18-year-old Jamsai Unsri expected to hear when he went in for his annual physical was that he had a hole in his heart. See how cardiothoracic surgeon Makoto Hashimoto, M.D., at Baptist Health Cardiac & Vascular Institute used highly advanced robotic surgery techniques to repair the hole so that Jamsai could graduate from high school and start college this fall. Video by Eduardo Morales..)
Confirming the Diagnosis of ASD
Jamsai was referred to Paula Montana De La Cadena, M.D., a cardiologist at Baptist Health Miami Cardiac & Vascular Institute, who was able to confirm his ASD diagnosis.

Sirikorn “Jamsai” Unsri
“I first met Jamsai in October 2024 after a referral by his pediatrician, who had detected an abnormal heart sound called ‘fix split S2,’ which is highly suggestive of ASD,” Dr. Montana recalls. “I confirmed the suspected diagnosis of ASD with a trans-esophageal echocardiogram and a cardiac MRI.”
Jamsai had the most common atrial septal defect – the ostium secundum – which Dr. Montana says represents 75-80% of all ASD cases. It is also one of the most frequent congenital heart lesions found in adults, who make up 30-40% of ASD cases.
A Father’s Worst Fear
The news hit his parents hard – especially his father, Minesh Mehta, M.D., a renowned radiation oncologist, chief of radiation oncology at Baptist Health Miami Cancer Institute and chair, Department of Oncological Sciences, Florida International University Herbert Wertheim College of Medicine. Though a physician with decades of experience treating patients with cancer, nothing prepared him for hearing that his own son’s heart needed major surgery.
“This was really an unbelievable diagnosis – it felt like a ton of bricks had landed on us,” Dr. Mehta admits. “Jamsai was healthy physically and emotionally and very active. In fact, he had just started working out and was going to the gym and lifting weights. Suddenly we were told he had a large hole in the heart – a life-shortening condition requiring a significant surgical procedure. It was traumatic and frightening for all three of us.”
The Best Care, Right Here at Home
True to his medical training, Dr. Mehta immediately began researching every possible option for Jamsai. He and his wife reached out to top cardiac centers across the country, interviewed physicians and weighed different procedures to repair their son’s ASD. At first, they assumed they would need to leave Miami to get Jamsai the surgery he needed.
But the more they compared outcomes and studied options, the more one conclusion became clear: for the best shot at a successful outcome for their son, they wouldn’t need to leave Miami. The expertise needed to perform this exceedingly rare and delicate robotic surgery was available in his own backyard, at Baptist Health Miami Cardiac & Vascular Institute.

Makoto Hashimoto, M.D., cardiac surgeon at Baptist Health Miami Cardiac & Vascular Institute
“Sometimes you don’t need to search across the country—the best care, the best team and the most humanity can be found right here at home,” Dr. Mehta says. “As my wife and I got deeper into our research, it quickly dawned on us that Miami Cardiac & Vascular Institute was the best place in the country for the type of procedure Jamsai needed. It had the outcomes, the techniques and, most importantly, the humanity behind the robot.”
The Right Surgeon for the Job
The family met Makoto Hashimoto, M.D., cardiac surgeon at Miami Cardiac & Vascular Institute and professor and director of robotic cardiac surgery at Florida International University Herbert Wertheim College of Medicine. An internationally trained surgeon, Dr. Hashimoto is a world-renowned robotic cardiothoracic surgeon and a pioneer in using robotic techniques to treat both congenital and acquired heart disease.
“When I first met with Dr. Hashimoto, I realized that he’s a superb individual, very accomplished and obviously very highly skilled,” recalls Dr. Mehta. “But he’s also a father like me and so he could put himself in my shoes. He could approach me as a father, as if it were his own kid’s life on the line.”
For Jamsai, meeting Dr. Hashimoto eased his anxiety. “My first impression was that he was extremely calm and collected,” he recalls. “He explained the diagnosis, the surgery and the recovery. He didn’t talk to me like just another patient, he spoke to me as a person. That connection meant everything.”
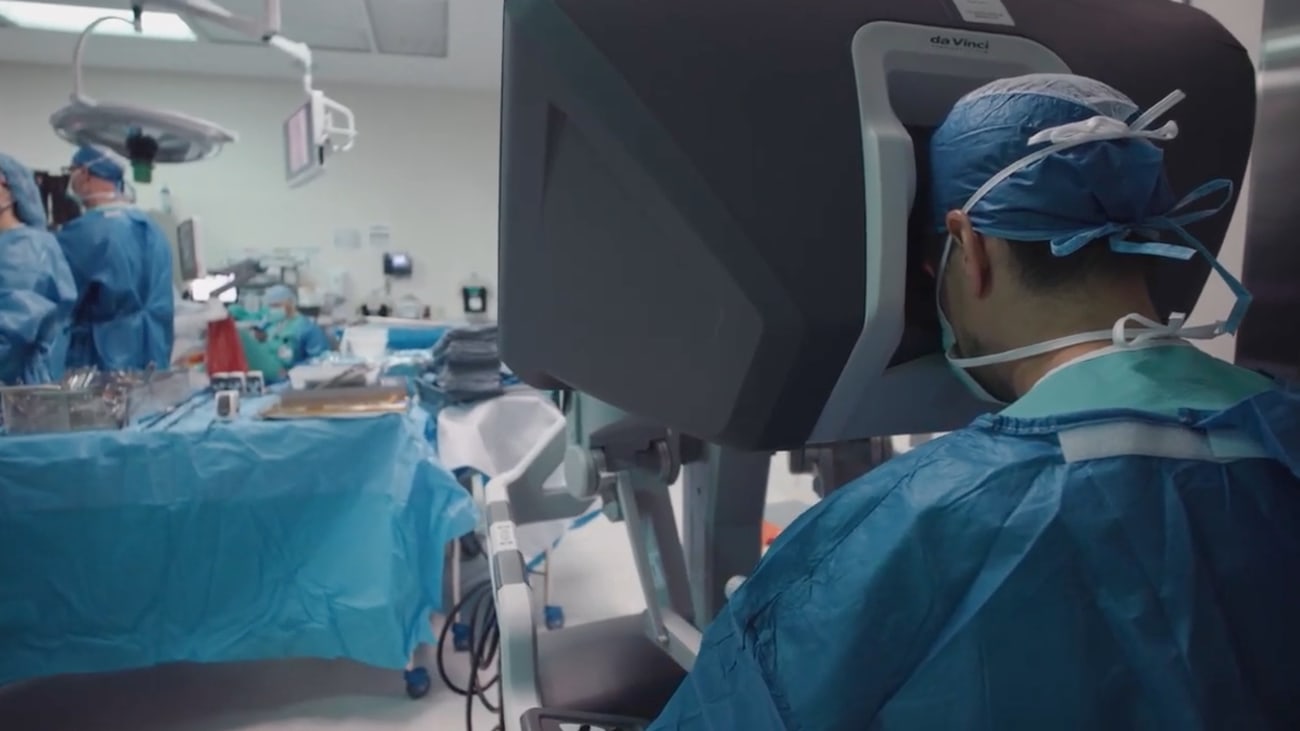
Instead of opening the breastbone to access the heart – a procedure called a sternotomy – Dr. Hashimoto and his team use a highly sophisticated robotic surgery system to perform delicate operations through tiny incisions between the ribs. For Jamsai, this approach meant avoiding traditional open-heart surgery that requires more extensive recovery. Instead, his ASD would be closed with a robotically inserted patch.
A Rare Procedure by a Skilled Surgeon
Robotic ASD repair is not very common worldwide, according to Dr. Hashimoto. Last year, only about 14,000 robotic heart surgeries were done worldwide; of those, he says, only 2% were for congenital heart disease such as ASD.
Patients requiring robotic ASD repair are typically older, notes Dr. Hashimoto, adding that Jamsai was one of the youngest patients he’s operated on using this procedure.
“It is a rare procedure but the concept is simple: we want to close that hole,” Dr. Hashimoto says. “But to do so, we must stop the heart, using a heart-lung machine, then patch the hole with a tissue product called a pericardium patch.” Once repaired, the result is lifelong, he says, and patients are able to do everything they want to do.
Miami Cardiac & Vascular Institute now performs the largest number of robotic heart surgeries in the region, according to Dr. Hashimoto, but for him, the focus is never just on technology. “Robotic surgery is a collective effort, with the surgeon and the entire surgical team working together – many of them behind the scenes – to make sure the patient gets the very best care possible.”
The Benefits of Robotic Cardiac Surgery
Dr. Hashimoto says the advantages of robotic cardiac surgery for both patient and surgeon are clear. With the robotic surgical system, he can perform very precise operations through a small incision in the right chest, using tools that can move with extreme dexterity and precision.
“My hand movements are seamlessly translated into precise, real-time movement of multiple instruments, which actually provide a better degree of motion than the human hand can,” Dr. Hashimoto explains. “And we have a magnified view – more than ten times greater than the human eye.”
From the patient’s perspective, robotic cardiac surgery avoids having to cut open the breastbone, or sternum, which Dr. Hashimoto says reduces complications and helps speed recovery. “Patients who have robotic surgery typically experience less pain and have shorter hospital stays and a quicker return to daily life,” he says.
A Worried Father’s Vigil
Hours after his surgery, Jamsai woke up and learned his surgery had been a success. “At first, it felt like nothing had happened, like it was a dream,” he recalls. But then the reality set in. “The recovery was painful. I had to hug a pillow every time I coughed. But the team checked on me constantly, every half hour.” That gave him strength to keep pushing through his recovery, he says.
While Jamsai recovering, Dr. Mehta wrestled privately with his own emotions. “As a father, I had to be the rock,” he says. “My wife was anxious, too, and I didn’t want my son to see my fear so I hid it. But when I was alone, I second-guessed everything. Had we made the right decision? Should we have gone elsewhere?”
One Sunday morning, the answer came in the form of an unexpected visit while Dr. Mehta was with his son, who was still recovering in the hospital. Instead of a nurse practitioner or junior physician coming to check on Jamsai, it was Dr. Hashimoto himself, Dr. Mehta recalls.
“When I asked why he was here on a Sunday, he gave me a puzzled look and said, ‘Why do you ask me that? My patients are my responsibility.’ That’s when I knew, without a doubt, that we had made the right choice.”
Jamsai was discharged a few days after his surgery. Within weeks, he was back to walking, exercising and even going on his first post-surgery date. “That moment was so emotional for me, I cried,” he admits. “I felt like I had my life back.”
New Perspectives for Both Father and Son
Dr. Mehta says Jamsai’s journey reinforced not just his role as a father, but as a physician.
“As physicians, we often keep distance from our patients – it’s a defense mechanism. But when your own child is the patient, that distance disappears. You gain empathy and compassion in ways you never imagined.”
Another thing both he and Jamsai learned, Dr. Mehta says, is how essential healing arts like music and creativity are to a patient’s recovery. “At Miami Cancer Institute, we have the Arts in Medicine program, in which visual and musical artists engage with patients to comfort and soothe them, distract them or simply to help them pass the time.”
Jamsai, a classically trained pianist who has always wanted to become a doctor, volunteered for the program and regularly played piano for those cancer patients. He says it was “truly one of the most life-changing experiences I’ve had.”
“I would just be playing and a patient would come up and tell me their life story, sharing with me what they’ve been going through, telling me how great their care has been at the Institute. That experience has developed both my character and my knowledge of how patients interact with the medical environment around them.”
His father says that playing for cancer patients “became a part of Jamsai’s own healing” and that the experience influenced him as well, reinforcing his belief in the value of humanity in medicine.
“Medicine is not just all about procedures and machines and tools and techniques and robots,” he declares. “It’s also about the humanity and the compassion and the person behind the robot.”
For Jamsai, his ASD surgery became a turning point in his life’s direction. “Being a patient gave me a new perspective on medicine,” he says. “I saw the complexity behind the scenes and the humanity it takes to care for someone. I want to become a physician myself one day — maybe even a cardiothoracic surgeon like Dr. Hashimoto.”
Even Better and Stronger Than Before
Today, Jamsai says he feels better than ever. “I’m at 110% now,” he says with a smile. “Maybe it’s a placebo effect or maybe it’s just that I’m getting more oxygen.”
He admits that right after his surgery he was “completely devastated” because his voice was gone. “In addition to being a pianist, I’m also a singer so I was wondering if I would ever be able to sing again,” he says. “Now I can sing better than ever and I have regained the ability to exercise, to work out and to run like normal again. The results of my surgery have been truly impactful.”
Dr. Hashimoto takes quiet pride in seeing his young patient thrive. “Robotic surgery offers fast recovery, precise outcomes and fewer complications,” he says. “That’s a huge benefit for a young man like Jamsai who is just starting college and has a full life ahead of him.”
And for Jamsai, the experience that once rattled his world now fuels his dreams. With his heart healed and his future wide open, he just started his first year of his college pre-med program. He says perhaps one day he’ll have an opportunity to train under Dr. Hashimoto.
“Every physician I’ve encountered at Baptist Health was extremely accommodating, welcoming and amazing,” Jamsai observes. “If I end up in cardiothoracic surgery, I would love an opportunity to train with the surgeon who saved my life.”
Click here to learn more about the physicians and services available at Baptist Health Heart & Vascular Care.

